
Presentation at 2023 clean indoor air expo
Using Clear Public Health Messaging to Break Barriers to Infection Prrvention
by Shea O'Neil
October 2023
Supporting Document:
Clear Public Health Messaging: A Step Beyond the Swiss Cheese Model:
How Do the Layers Actually Work and How Do They Interact?
By Shea O'Neil, last edited 4-24-24
Supporting Document for the Presentation at the 2023 Clean Indoor Air Expo, Printable Google Doc Version here
The Urgent Need for Clear Public Health Messaging
One of the biggest roadblocks to the goal of reducing infections, slowing viral evolution, and subsequently reducing chronic disease, disability, healthcare strain, premature deaths, and economic blights (i.e. short-term costs, hospitalization costs, long COVID costs, and mortality costs) has been the confusing and often conflicting public health messaging on how to use the tools effectively to prevent COVID-19 infection.
Figure 1: Clear Messaging
There is currently a scientific consensus [1] that one of the most significant modes of transmission for SARS-CoV-2 is through aerosols generated when we breathe and talk.
[1] Scientific Consensus: Aerosol spread has been acknowledged by both the WHO and the CDC. The CDC published a study demonstrating “the high transmissibility of Omicron variants… even across rooms and floors” in a hotel. Since then many studies have been done confirming aerosol-spread COVID-19, including studies on outbreaks and studies using viral genomic sequencing to determine sources, such as a study in which a single patient transmitted SARS-CoV-2 to six healthcare workers (HCW) who were wearing surgical masks (which are made for protection from droplets), as opposed to N95 respirators (made for aerosol protection) as well as spreading it to three other patients. This study noted all the HCWs also wore eye protection and that three of the HCWs had no direct contact and maintained a distance of at least 6 ft from the infected patient. In a real world study on the efficacy of respirator masks in a COVID ward, when surgical masks were replaced with FFP3 (N95) respirators for nurses on a COVID-19 ward, infection risk declined by 52%-100%. A 2021 review of airborne transmission published in Science highlights the number and viral load of aerosols produced through speaking and other expiratory activities are much higher than those of droplets, and they can reach further into the lungs, again affirming aerosols as the primary way COVID-19 is transmitted. A 2021 Lancet analysis of research supporting airborne transmission points out that smaller aerosols showed higher pathogen concentrations than droplets, can linger in the air for hours as well as travel through air conditioner ducts, and that “Reducing airborne transmission of virus requires measures to avoid inhalation of infectious aerosols, including ventilation, air filtration, reducing crowding and time spent indoors, use of masks whenever indoors, attention to mask quality and fit, and higher-grade protection for health-care staff and front-line workers.” According to the US Environmental Protection Agency (EPA): “Transmission of COVID-19 from inhalation of virus in the air can occur at distances greater than six feet. Particles from an infected person can move throughout an entire room or indoor space. The particles can also linger in the air after a person has left the room – they can remain airborne for hours in some cases. Someone can also be exposed via splashes and sprays of respiratory fluids directly onto their mucous membranes. Spread may also sometimes occur through contact with contaminated surfaces, though this route is now considered less likely.”In the 2022 Delphi Consensus published in Nature, a multidisciplinary panel of experts on COVID-19 from across the world contended, “Considering the airborne nature of transmission, governments should regulate and incentivise structural prevention measures, such as ventilation and air filtration, and high priority should be given to preventing SARS-CoV-2 transmission in the workplace, educational institutions and commercial centres.”
Additionally, the dangers of COVID-19 move beyond acute-phase infection, and have, for millions of people, developed into serious, long-term, chronic, disabling, and even deadly effects of long COVID [2].
[2] Long COVID, also referred to as post-acute sequelae of COVID-19 (PASC), has affected millions of people and can cause a wide range of serious complications including disability and death. According to a 2023 Nature article, “long Covid incidence is estimated at 10–30% of non-hospitalized cases, 50–70% of hospitalized cases and 10–12% of vaccinated cases …Symptoms can last for years, and particularly in cases of new-onset ME/CFS and dysautonomia are expected to be lifelong. With significant proportions of individuals with long COVID unable to return to work, the scale of newly disabled individuals is contributing to labour shortages. There are currently no validated effective treatments.” A 2021 systematic review found more than half of COVID-19 infections resulted in long COVID six months after recovery. Long COVID can result in long-term cardiovascular outcomes, gastrointestinal problems, multi-organ impairment, abnormalities of blood vessels and coagulation, mitochondrial dysfunction, functional impairment and fatigue, muscle abnormalities, immune dysregulation, detrimental neurological impacts (including brain cell fusion, depressive, and cognitive impacts), and increased risks associated with reinfections. A 2023 Nature immunological review concluded “The oncoming burden of long COVID faced by patients, health-care providers, governments and economies is so large as to be unfathomable, which is possibly why minimal high-level planning is currently allocated to it. If 10% of acute infections lead to persistent symptoms, it could be predicted that ~400 million individuals globally are in need of support for long COVID.” A 2023 Scientific American article stated “the most common, persistent, and disabling symptoms of long COVID are neurological”, later quoting a physician saying, “I now think of COVID as a neurological disease as much as I think of it as a pulmonary disease, and that's definitely true in long COVID.” Although formal guidance on how to record long COVID on death certificates was not released until 2023, CDC data from early 2024 has shown thousands of deaths of US citizens from long COVID. The only way to prevent long COVID is to prevent COVID-19 infection. Persistent infections- those that last longer than 30 days with replicating viruses– have also been implicated in the evolution of new viral variants, suggesting that reducing infections will also slow viral evolution.
Now that we know, we need to develop the appropriate public response and policy-making response [3]. We need to acknowledge where our messaging has gone wrong, where it was politicized, and back away from misinformation, anger, unwillingness, and confusion about the science.
[3] Public health policy response has not been updated in healthcare, workplaces, or schools around the world to align with prevention of aerosol spread viruses. In “Mitigating airborne transmission of SARS”, published in the The Canadian Medical Association Journal, the authors state, “Although good ventilation can mitigate long-range aerosol transmission of SARS-CoV-2, the WHO and CDC’s acknowledgement of airborne spread at close range highlights an urgent need to revisit PPE guidelines in all Canadian health care settings.” They point out that high-quality masks such as N95 respirators are currently required only for “aerosol-generating medical procedures”, despite studies that have shown that “exertional activities and coughing produce more aerosols than some aerosol-generating medical procedures”. They also point out that because SARS-CoV-2 can be spread by both short-range and long-range aerosol inhalation, ventilation needs to be combined with the known guidance that “recognizes that N95 respirators are the gold standard for protection against short-range aerosol inhalation.” They go on to say how these measures are important outside of healthcare settings as well, stating: “Although social measures such as paid sick leave are vital, standardized masks (ideally, fit-tested respirators) are still a critically important protective measure.” In the US, the CDC is currently reviewing infection control guidelines in healthcare, and current drafted guidance, although acknowledging N95 respirator masks provide superior infection, call instead for surgical masks requirements and do not include ventilation or filtration guidelines. Similar concerns have been raised to the NHS regarding updates to the Infection Control Manual in England by the British Medical Association. And, according to a multinational Delphi Consensus to end COVID-19 as a public health threat, a panel of 386 academic, health, non-governmental organization, government and other experts in COVID-19 response from 112 countries and territories were in near-unanimous agreement that “SARS-CoV-2 is an airborne virus that presents the highest risk of transmission in indoor areas with poor ventilation. Risk-related communications from all actors should clearly emphasize that transmission of SARS-CoV-2 is primarily caused by inhalation of the virus.” Furthermore, they stated: “vaccination alone will not end COVID-19 as a public health threat. Infection rates tend to increase when governments discontinue social measures, including non-pharmaceutical interventions, regardless of the level of vaccination. Thus, all countries should adopt a vaccines-plus approach, including a combination of COVID-19 vaccination, other prevention measures, treatment and possibly financial incentives.”
As we have seen at events such as the 2023 Clean Indoor Air Expo, the technologies exist, the impetus exists, and the science and research into COVID-19 transmission and long-term effects of COVID-19 exist. Yet, having the tools available is one thing, and getting people to use them effectively is another. This can be helped with clear public health messaging.
Reducing Infections with Clear Public Health Messaging
Two properties about protections from infectious diseases are important:
(1) Defining individual and societal responsibilities, and
(2) Describing the type, level, and combinations of protections needed to effectively to prevent infections.
Let’s take a closer look at how we can use clear public health messaging for each of these properties to reduce transmission.
Shared Individual and Societal Responsibilities
The responsibilities of implementing protections from communicable diseases are shared between individuals and societies, and cannot be assessed as an individual responsibility alone. This is because the decision of one individual to engage with risk may limit the ability of other individuals to protect themselves. When risk is shared, mitigation efforts require collective action to succeed. Typically, the more society does to mitigate a risk, the less of the burden falls onto the individual. However, neither of these entities can be successful acting alone. This notion runs contrary to the "You do you" approach that has become popular amongst public health agencies, that places the burdens and responsibilities solely on individuals.
Figure 2: Shared Individual and Societal Responsibilities

Water safety is a good example of how society manages collective responsibility for a shared risk. How well a government develops and implements water safety standards, how well municipalities monitor and test water, how well responders report incidences of contamination, are all important factors impacting how effectively an individual is able to protect themselves. The individual is responsible for responding to messaging to disinfect or avoid the tap water when directed, as well as to take everyday precautions when handling water to reduce contamination risks.
No lone entity can maintain the full burden of responsibility for shared risks. When it comes to COVID-19, both individuals and groups in society need to be aware of the risk that exists, how the protections work, why they are necessary, and why widespread participation provides the best chance at success to effectively prevent transmission and infection. Part of this is understanding how the layers of protection actually work, and incorporating both the combination of layers as well as the level, or strength, of each layer to use them successfully.
What are the Layers of Protection?
In this paper, we talk about protections in terms of “layers” and “levels”. The layers of protection are the actions that can be taken to prevent the spread of disease from an infected individual to someone without an infection. For a disease like COVID-19 that transmits through the air, these layers include:
Having households avoid being with other households in the same spaces, i.e. homes, schools, workspaces. Protection: Remote (ie virtual options, curbside pickups, delivery)
If people need to be together, then the space itself has to be safe for people to be together. Protections: Masking, physical distancing, air filtering, ventilation, symptom screening, properly testing, properly isolating.
Finally, as a backup, we can help people who are infected better protect themselves biologically from the effects of the infection. Protections: Vaccination, treatments
Let’s take a look at some models to see how these layers of protections work together in different ways to reduce infection and transmission risks.
The Need to Move Beyond the Swiss Cheese Model
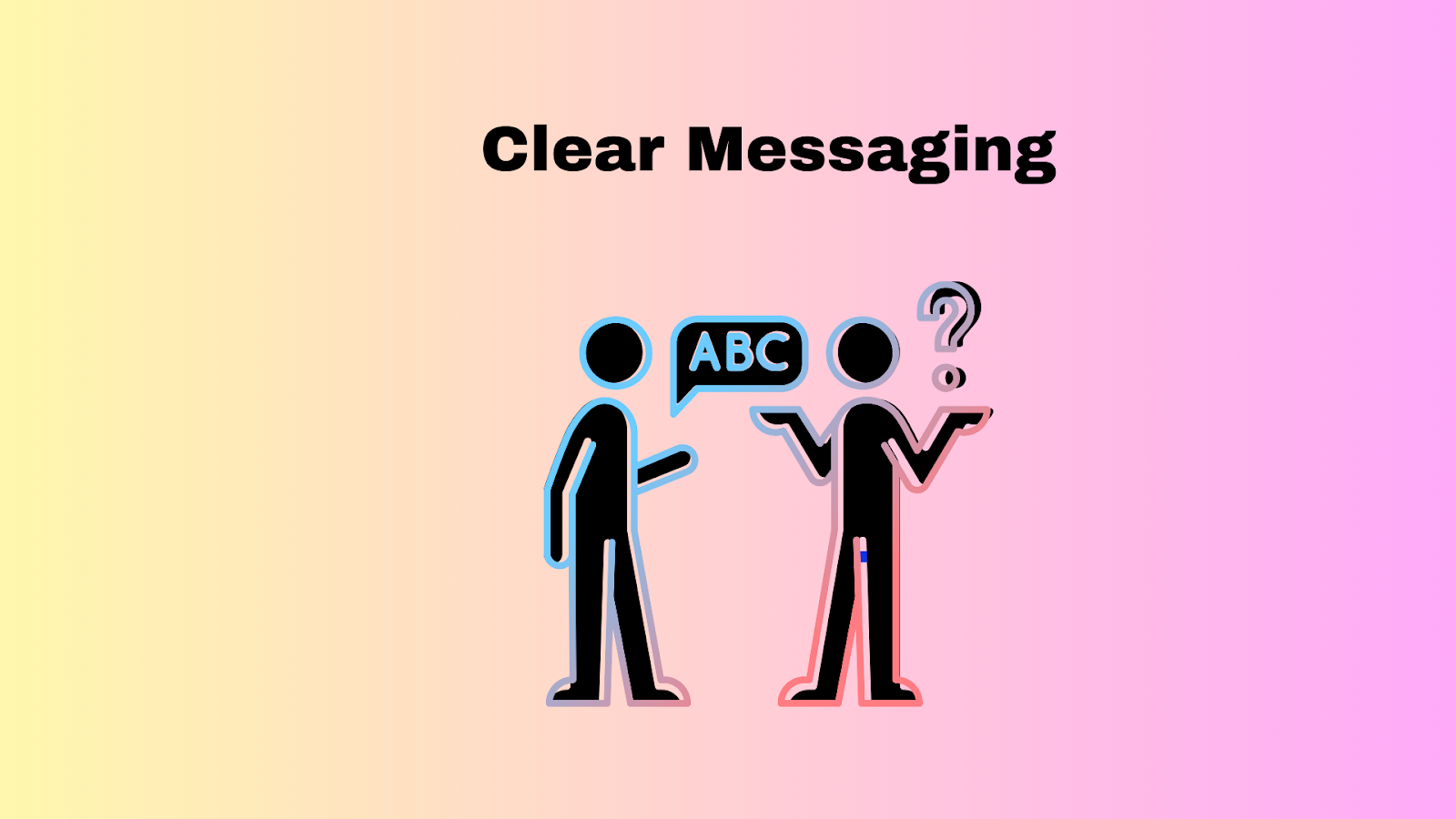
The Swiss Cheese Model is a popular way to describe a multi-layered approach to COVID-19 prevention. In this model each protection, or layer of prevention, constitutes one piece of swiss cheese, and its weaknesses are represented as the holes. We can stack the slices of cheese (preventions) to reduce the chances that something (COVID-19) makes it through the holes (exposure leading to infection).
Yet, the Swiss Cheese Model has two important limitations. First, it fails to account for the differences in the amount of protection each layer offers. It also ignores how each layer’s strengths and weaknesses interact when combined with other layers.
Figure 3: Weaknesses in Using the Swiss Cheese Model
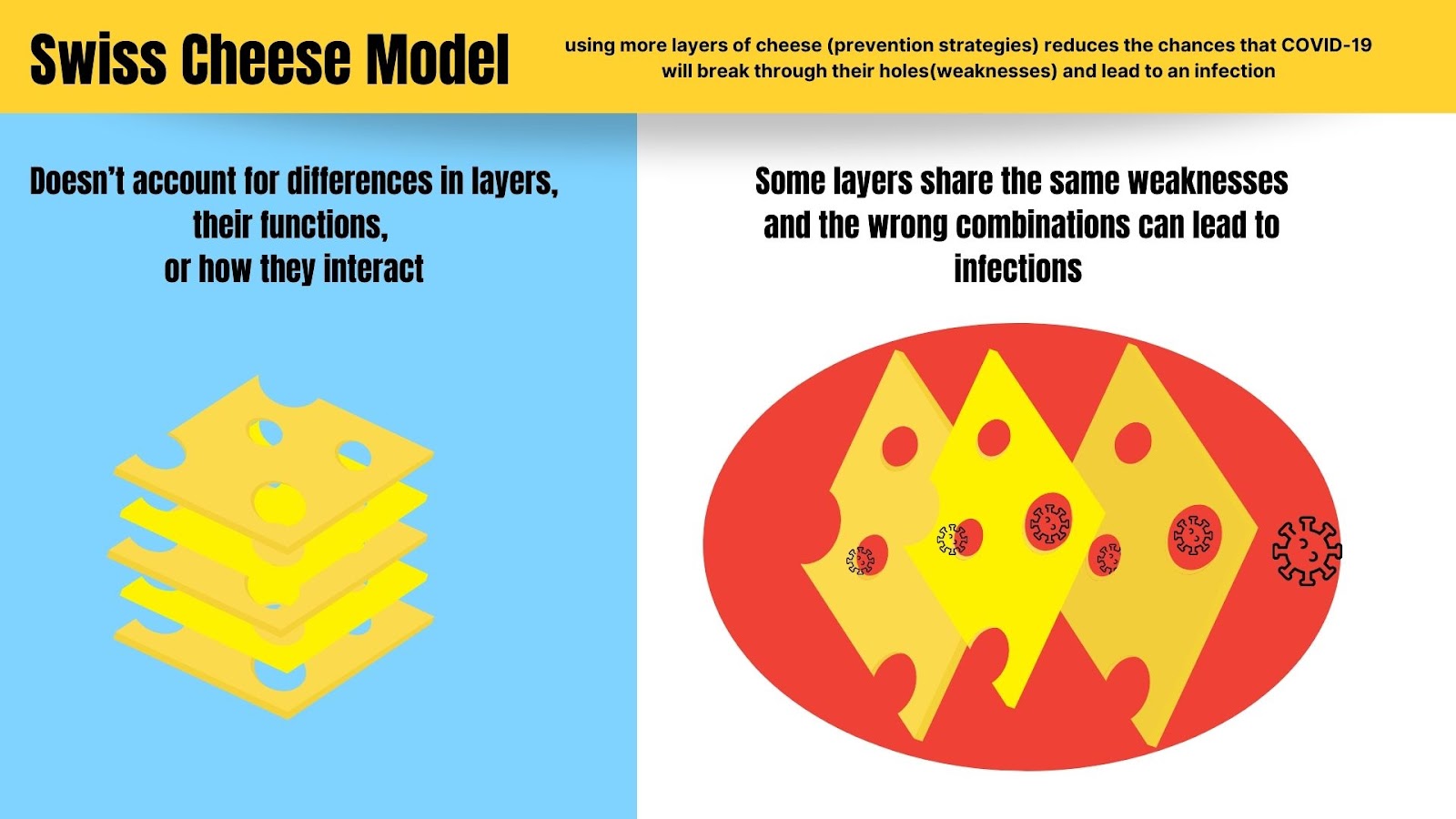
Figure 3 Description: In the Swiss Cheese Model, the layers of protection for COVID-19 are all viewed as having the same amount of holes (weaknesses). It does not describe how the holes (weaknesses in layers) might line up in certain combinations and lead to infections.
For instance, if the slice of cheese representing masks has the fewest holes and we remove it from the stack, our remaining slices (let’s say, air filtration and testing) could have holes that line up, and therefore let through an infection. This is because tests and air filtration have limitations that other protections like masks do not. Testing with a Rapid Antigen Test can lead to false negatives in many cases, sometimes nearly half, allowing an infectious person to enter a space. Air filtration takes time to clear the air and does not prevent an infectious dose of the virus from moving through the air from one person to another while they are talking without masks on. Those layers at those levels do not protect adequately.
Figure 4: A More Accurate Portrayal of the Differences in Layers
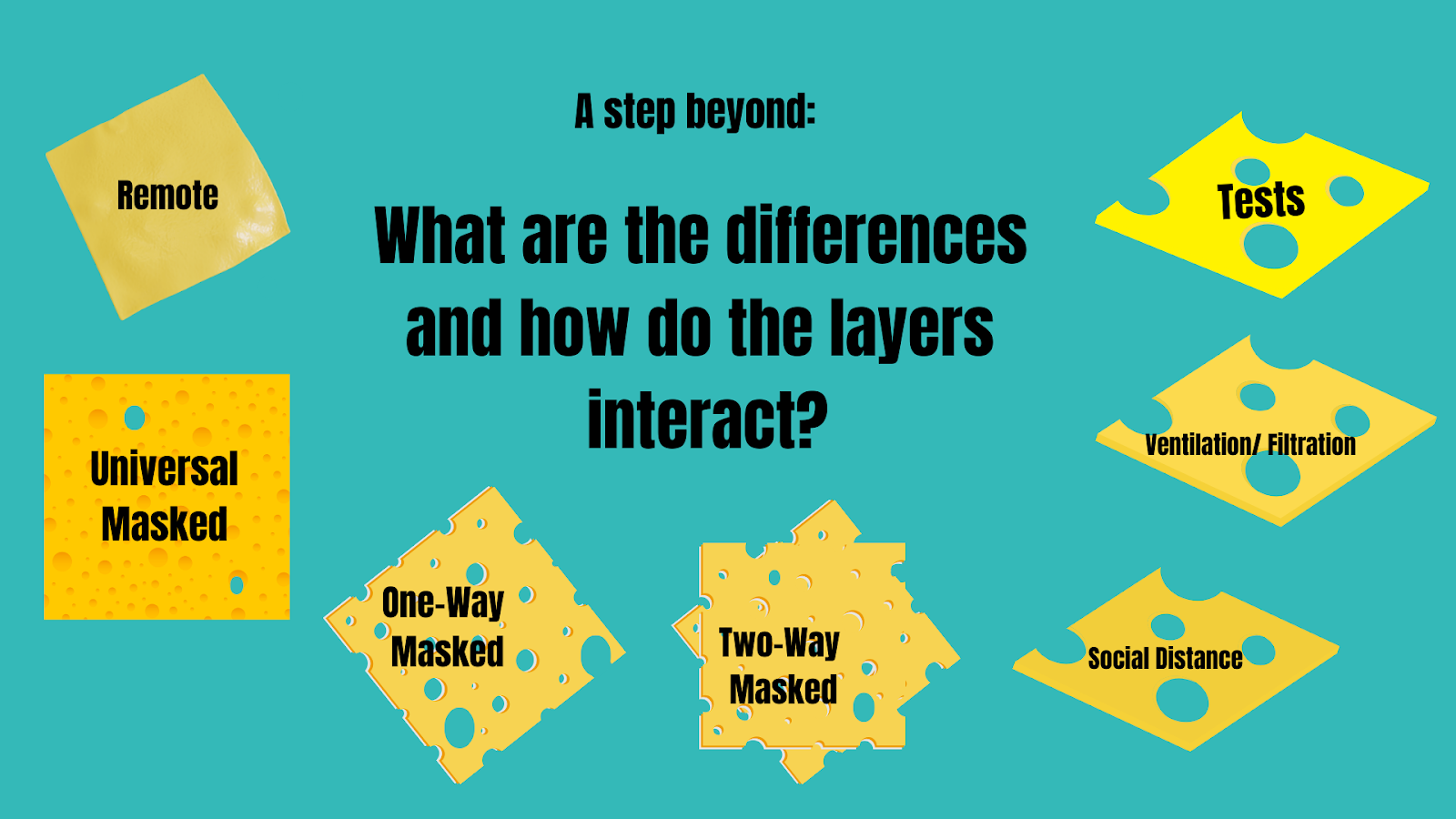
Image Description: Since the layers of protection for COVID-19 can be very different from each other in the amount of protection they offer, Figure 4 above would be a more accurate picture. For example, remote (when people are interacting virtually from their home environments) offers no chance of transmission, so the cheese has no holes. Masks have fewer vulnerabilities when used universally than when only used by one person. Tests, ventilation/filtration, and social (aka physical) distance have weaknesses that could line up with each other leaving an individual open to infection if they are not masked.
Clear public health messaging needs to communicate how we can use different layers, different levels of the layers, and correct combinations of the layers to provide protection from infection.
What are the Levels of Layers?
It is important to recognize that each of the layers also can be applied at different levels, and those levels offer different degrees of protection. The 5 Pillars of Protection model gives three levels for all but one of the layers, which it conceptualizes as pillars rather than slices of cheese.
The 5 pillars and their levels include:
Masking
Level 1: N95,
Level 2: P100 Respirator,
Level 3: PAPR
2. Air Quality
Level 1: 6 ACH (Air Changes per Hour),
Level 2: 12 ACH,
Level 3: Analyzing Air flow
3. Social/ Physical Distancing/ Remote
Level 1: Maximize physical space between people
Level 2: Hybrid Remote,
Level 3: Fully Remote
4. Testing
Level 1: Twice weekly testing with RAT or NAAT;
Level 2: Daily testing with NAAT;
Level 3: Twice daily with NAAT
5. Vaccination: up-to-date
Figure 5: The 5 Pillars of Protection
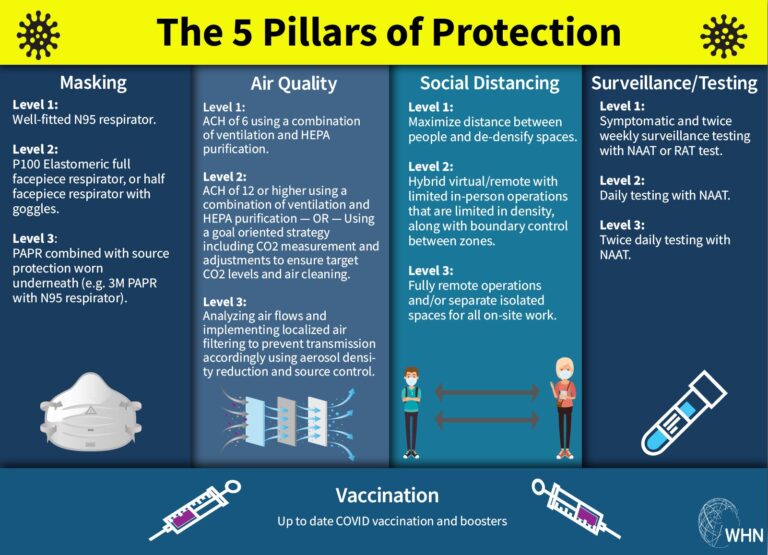
Image Reference: The Five Pillars of Protection and their levels, by the World Health Network
The concept of the 5 Pillar model is that if there is a weakness in one pillar (or layer), increasing the levels of other pillars will help accommodate for the weakness. For instance, if you were in a setting with air quality at less than level 1 (which is 6 ACH), you could raise the levels of other layers (i.e. increase masking level from N95 to a P100 elastomeric; increase physical distancing to hybrid virtual options; increase testing to daily testing with NAAT.) A weakness in the model is that it does not define how to find correct layers, levels, and combinations that work to reduce infections.
Masking: An Essential Layer
As stated earlier, not all layers of protections are equal in the amount of protection they provide, and none of the layers is sufficient on its own. One of the first layers many people try to drop when using a multi-layered approach is a respirator mask.
However,
Most other layers of protection are not sufficient on their own to prevent infections, and need to be used in combination with masks to best reduce infection risks. Respirators, such as N95 masks and further described in this work as “masks”, offer source control that is unachievable by other means. Masks can directly filter the air as it is exhaled from a possible source (when the source is masked), and again before you breathe it in (when you are masked) thereby significantly reducing transmission of infectious aerosols, including COVID-19 [4].
[4] Masks work: A pre-COVID study showed respirator masks significantly reduced infections with airborne pathogens, also showing continuous use of respirators to be more effective than intermittent use. A 2021 report published in Science concludes facemasks effectively limit the probability of SARS CoV-2 transmission, while also acknowledging that mask efficacy depends on airborne viral load, adequate fit and filtration, and is increased with using other protections to reduce viral load. As mentioned earlier, in a real world study on the efficacy of respirator masks in a COVID ward, when surgical masks were replaced with FFP3 (N95) respirators for nurses on a COVID-19 ward, infection risk declined by 52%-100%. A study published in PNAS showed with only the susceptible wearing a surgical mask, the upper bound of infection risk is 90% after 30 minutes. However, when both the susceptible and infected wear a well-fitted respirator mask, the risk is 0.4% after an hour. A 2022 research article titled “Mask wearing in community settings reduces SARS-CoV-2 transmission” found that the mean observed level of mask wearing corresponded to a 19% decrease in the reproduction number, and stated that “the evidence that mass mask wearing reduces transmission implies that mandates (and other mask-promotion policies) may be effective against COVID-19 if and when they improve or increase the use of masks.” A 2021 study showed universal masking is significantly better than one-way masking. A 2022 study published in the Journal of Infectious Diseases found that fit-tested N95 mask combined with a portable HEPA filtration system offers the best protection against viral particles in the air.
Because studies show that much of SARS-CoV-2 transmission is from asymptomatic or presymptomatic carriers, it is important to mask when around others outside your household, whether you/they are experiencing symptoms or not [5].
[5] Asymptomatic and Symptomatic Transmission of COVID-19: According to a 2023 study, transmission can happen in as little time as 20 seconds to 4 minutes (depending on whether it's a high shedder or average shedder), and high levels of infectious virus were detected in exhaled breath regardless of vaccination status, with significant amounts emitted even in mild and asymptomatic cases. A Nature study from December 2023 also showed transmission can happen in as little as a few minutes in normal indoor environments. A 2022 systematic review on transmission concluded: “High-quality studies provide probable evidence of SARS-CoV-2 transmission from presymptomatic and asymptomatic individuals.” A 2021 study using data from infector-infectee pairs found high infectiousness immediately prior to symptom onset. And, in a study published in JAMA in 2021, an analytical model found transmission from asymptomatic individuals was estimated to account for more than half of all transmissions.
When wouldn't Masking be prescribed?
While you are working remote/ virtual from your home
For children under the age of two (24 months)
For those who have certain disabilities, who are unable to safely wear a mask due to that disability.
For those who are in medical situations in which it is medically contraindicated to wear a respirator mask.
Finding the Respirator Mask that Works Best For Your Situation
You should try out different kinds of respirators such as N95 masks to find the best fit and comfort. There are many masks that allow for greater breathability, have see-through windows, are latex-free, and come in a variety of sizes and styles. Environment, activity level, and time can also be modified to find compatible adaptations. There are also N95 masks without metal in them for use in certain medical situations.
Figure 6: Respirator Masks, Like People, Come in Many Shapes and Sizes
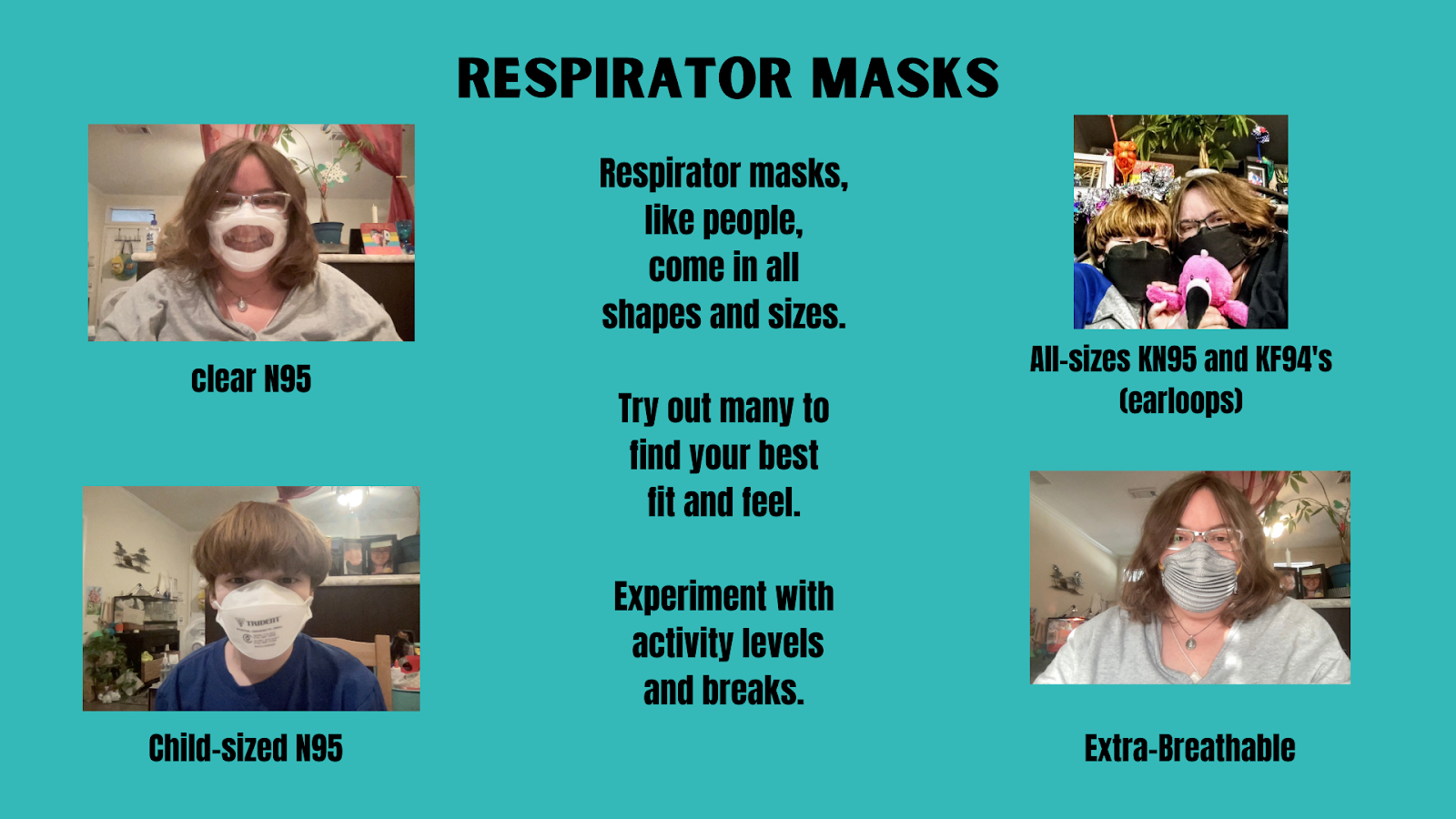
Figure Description: There are clear N95 masks for those who need to see mouths (top left photo), child-sized masks for children 2 and above (bottom left photo), KF94 with adjustable ear loops for adults and children (top right photo), N95 masks with folds that increase airflow for adults (bottom right, adult size pictured) and smaller sizes for adults with small faces and children (not pictured, but same design).
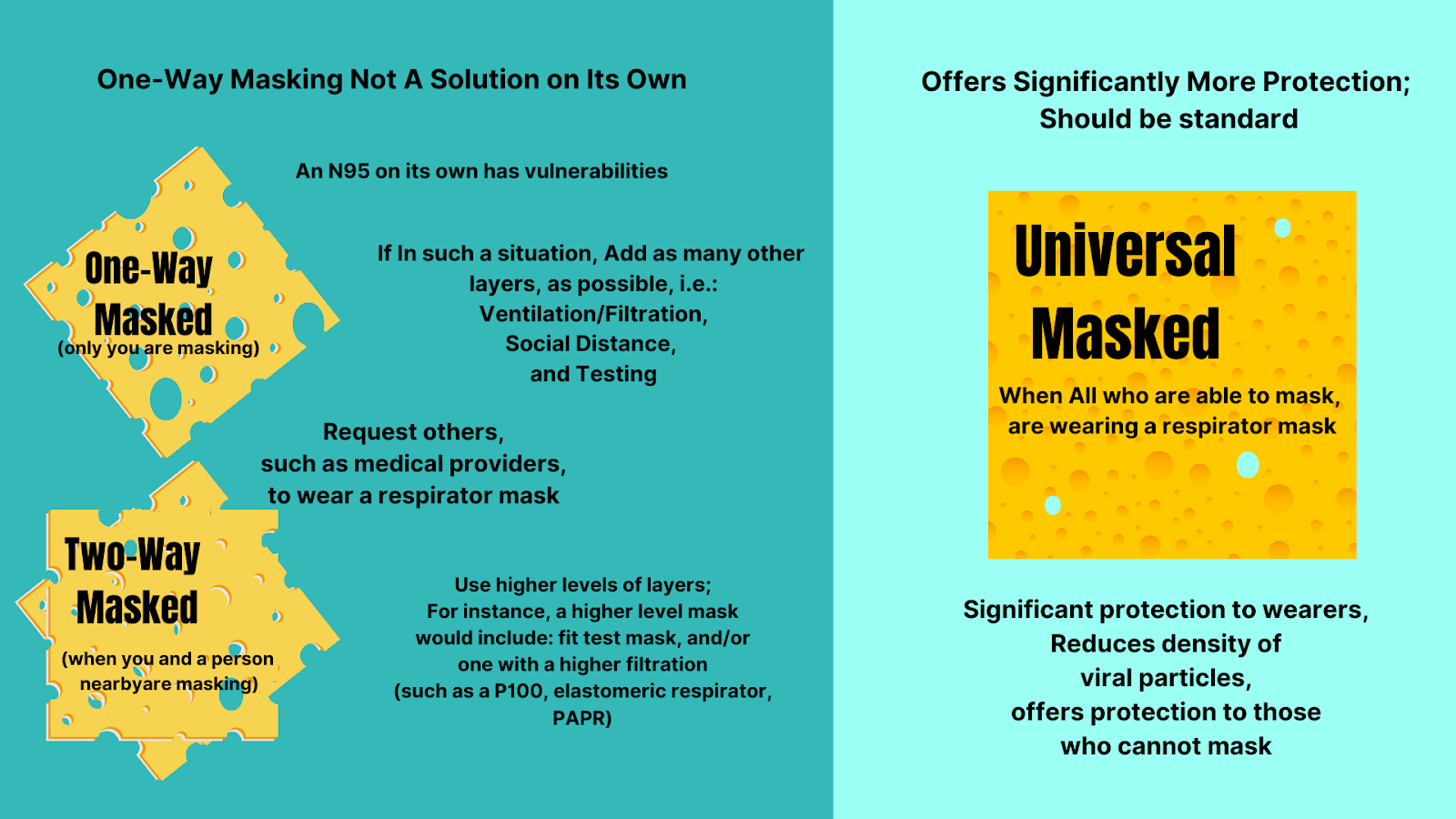
Is Masking an Individual Responsibility or a Collective Responsibility?
Masking is both an individual and collective responsibility because COVID-19 is a shared risk. When you have individuals in society who cannot mask (infants, those with certain disabilities or medical conditions), it is even more important that those around them ARE wearing a respirator mask, alongside other layers of protection. The more people who are masking in a space, the lower the risks of COVID-19 transmission, and the more protection offered to all– including those who cannot wear a mask.
It is also worth noting that one-way masking offers very limited protection, regardless of your individual risk profile. Universal masking offers significantly more protection than other masking situations.
One-way masking (when you are the only one masked) will require more layers of protection and/or higher levels of protection than two-way masking (when you and a person nearby are masking) or in universal masking (when all are masking) situations. If you find yourself in an unavoidable non-universal masking situation, you will want to take additional precautions. For example, you can improve your mask’s efficiency by finding one with a better fit, or with a higher level of filtration, (examples: fit-tested N95, elastomeric respirators, and PAPRs). You can also ask for others, such as medical providers and those interacting with you, to mask with N95s and use other reasonable accommodations to reduce exposure.
Figure 7: The Differences Between One-Way, Two-Way, and Universal Masking
Using Supporting Layers to Create Safe Shared Spaces
Shared spaces are any spaces where multiple households come together. They include public spaces such as schools, libraries, post offices, city centers, courthouses, etc. They also include private businesses and homes when multiple households gather there. Outdoor venues are considered shared spaces, since COVID-19 can spread outdoors (although outdoors does have an advantage of the layer of good ventilation, it is also affected by other factors such as the density of people in that space).
Shared spaces can be made safe by a combination of 2 factors:
1- reducing the amount of virus coming into a space, and
2- filtering the remaining virus out before it is breathed in by people in that space.
Figure 8: Reducing Viruses Coming In, Filtering Out Viruses That Do Get In
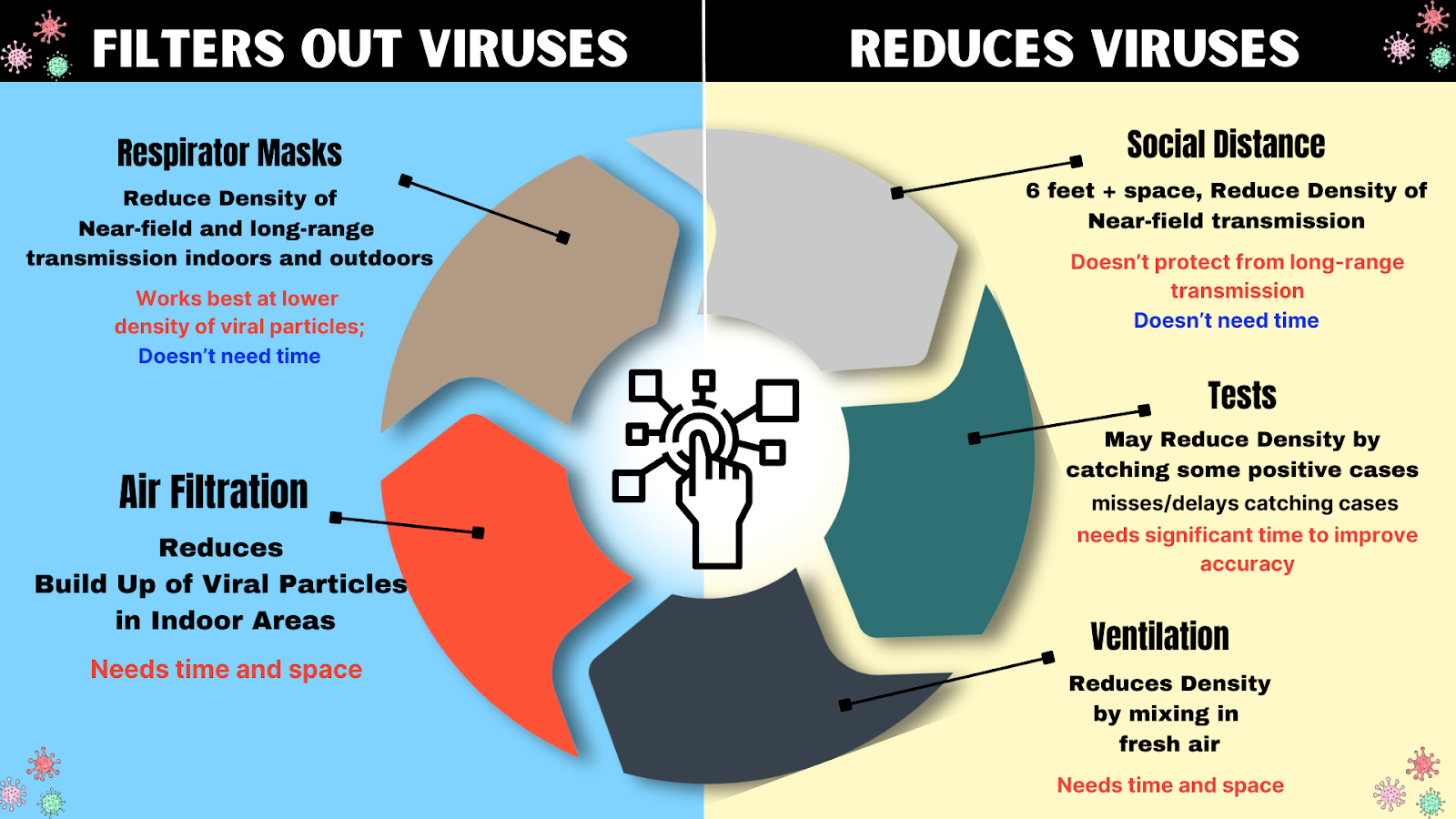
The combinations of certain layers of protection help to account for others’ weaknesses. For instance, masks work better at lower density of particles. Since viral particles are higher near the source, physical distance from the source can lower viral density, and thus compliment masks.
Air filtration and ventilation reduce long range transmission, but, because they require time and space to clear out the virus, they have a gap in protection that a mask can fill with its immediate protection.
Testing will reduce the chances of an infectious person coming into a space, but because tests require multiple tests over the course of days to provide accurate results and miss positive cases, in most cases they can only be used to reduce some viral load, again needing other layers to fill in the gaps in protection from missed cases, such as masking and filtering the air.
Protections such as social/physical distance, testing, and ventilation reduce the amount of virus coming into a space. Protections such as masking and air filtration filter out viruses. Both are important and complementary methods of reducing infection risks.
Supporting Layer: Adequate Ventilation and Filtration
Enhanced ventilation and filtration to the 6-12 Air Changes per Hour (ACH) range, in addition to masking, is recommended for the purposes of infection control, leaning towards the higher end when higher numbers of people are present in the space. Viruses like COVID-19 that can spread through aerosols can travel far through the air, remain infectious for hours, and transmit illness to others. Such infections can be greatly reduced by adding enhanced ventilation and filtration [6].
[6] Enhanced Ventilation/Filtration: In a 2022 bioaerosol study on the infectivity of coronaviruses, researchers explained that saliva acted as a protective mechanism for the virus. They found at both 40% and 60% relative humidity, half of the airborne coronavirus particles were still infectious after aging for one hour, and that at 25% humidity, half of the original particles remained infectious for two hours. A 2023 study published in Nature researchers' data showed that “exhaled aerosols from a single person can transmit COVID-19 to others within minutes at normal indoor conditions.” A 2022 study published in the Journal of Infectious Diseases showed when combined with fit-tested N95 masks, gloves, and face shields, HEPA filtration provides protection against high viral loads over prolonged periods of time by reducing virus to near-zero levels. A 2022 systematic review of 11 studies also found HEPA purifiers significantly reduce airborne SARS-CoV-2 viral aerosols. HEPA purifiers and fan and Filter air cleaners such as the highly effective Corsi-Rosenthal Box (CR-box) have been shown to remove infectious particles and are recommended by CDC and NIOSH for reducing COVID-19. A 2022 study found using HEPA filters to the 7-12 air changes per hour can consistently remove SARS-CoV-2 and reduce viral load to below the detection limit, noting that because air does not pass through the air cleaner evenly, that it does require time, and that there are areas where the aerosols tend to linger, it should be combined with other measures. In a 2022 study researchers state: “Our analysis shows that mitigation measures to limit shared-room airborne transmission are needed in most indoor spaces whenever COVID-19 is spreading in a community. Among effective measures are reducing vocalization, avoiding intense physical activities, shortening the duration of occupancy, reducing the number of occupants, wearing high-quality well-fitting masks, increasing ventilation, improving ventilation effectiveness, and applying additional virus removal measures (such as HEPA filtration and UVGI disinfection). The use of multiple “layers of protection” is needed in many situations, while a single measure (e.g., masking) may not be able to reduce risk to low levels.”
In homes, ventilation and filtration is an individual responsibility. In public spaces it is a societal responsibility (although, in the absence of enhanced filtration or ventilation in a public space, individuals can attempt to compensate by bringing their own air purifiers).
Proper ventilation and/or filtration can be achieved by combining HEPA purifiers, CR box-style fan/filters, installing MERV 13 filters into HVAC systems, using mechanical ventilation, and/or opening windows. Tools such as Clean Air Stars, Rochester CADR Calculator, Smart Air CADR/ACH Calculator, or OHCOW Ventilation Calculation Tool are helpful in determining the type and number of purifiers to reach the appropriate air changes per hour for your space.
ASHRAE (American Society of Heating, Refrigerating and Air-Conditioning Engineers) has released standards for control of infectious aerosols in both 2021 and 2023. In ASHRAE Standard 241 (2023), it sets standards for the equivalent clean air flow rate, or the flow rate of pathogen free air into occupied areas of different settings that would have the same effect as the total of outdoor air needed to substantially reduce the amount of disease transmission in different settings [7].
[7] ASHRAE Standards: ASHRAE’s 2021 Ventilation for Industrial Settings During the COVID-19 Pandemic states: “Maintain between six and twelve air changes per hour (ACH), which will provide a greater than 99% purge in 30-60 minutes. This reduction applies when the building is unoccupied – the concept of purging does not apply if a source is still present (i.e., potentially infectious individuals are still in the workspace). It is important to maintain as much outside air and/or sufficiently filtered recirculated air as possible to achieve the goal of > 6 ACH.” The 2023 ASHRAE Standard 241Control of Infectious Aerosols, which can be previewed here, sets minimum equivalent clean air flow rates for infection risk mitigations for long range transmission according to the building’s occupancy category. In Table 5-1 they define spaces such as gym, classroom, lecture hall, classroom, health exam room, residential common space, etc and expresses the minimum equivalent clean airflow rate required using cubic feet per minute (cfm) per person as well as liter per second (l/s) per person to allow for better variation based on number of people in the room and activity level of the people. For a classroom setting it uses 40 cfm per person, or 20 l/s per persons, which for an average classroom of 25 it converts to approximately 8-12 ACH.
Ventilation and filtration need space and time to clear viruses out of the air. Masks give you protection in that space and time, while ventilation and filtration lower the density of infectious particles, making masks more effective.
One can use directed air flow, or blowing clean air (such as that from a handheld HEPA purifier) into your breathing space, to reduce chances of viral particles being in the vicinity. This can be especially important in situations where masking cannot be done, such as by a patient receiving dental work (for more information, see WHN’s Dental Safety Guide).
Supporting Layer: Social (Physical) Distancing
Social distancing, that is physically distancing people 6-10 feet apart, works as a supporting layer when combined with other layers, but does little on its own [8].
For one-way masking, personal space (6 feet) becomes even more important, as exhaled aerosol density is stronger closer to the source, and masks work better at lower viral density.
Physical distancing provides the space and time necessary for ventilation and filtration to start to clear infectious particles out.
Note: 6 feet is not a magic number. Infectious viral aerosols can and will travel beyond this distance, which is why wearing a mask is necessary even when spaced out.
[8] Physical Distancing: A 2021 study that looked at the combination of layers as opposed to each one singly, concluded that “Increases in ventilation rates, the use of HEPA air cleaners, the implementation of universal masking, and physical distancing can all play a role in decreasing the exposure of room occupants to airborne SARS-CoV-2. In this investigation, universal masking was the most consistent and efficacious mitigation strategy. Masking (the study used 3-ply surgical masks) reduced exposure by 50% or more compared to no masking. Ventilation reduced exposure by approximately 5% per 1 ACH increase, irrespective of whether increasing ventilation was achieved by increasing system HVAC or by the use of portable HEPA air cleaners. The placement of portable HEPA air cleaners was a factor in determining a Recipient’s exposure reduction. Nonetheless, the most effective portable HEPA air cleaner configuration was the use of two units at opposing sides of the room, e.g., one at the front and one at the back or one each at the sides of the room, or two units in the center of the room. Increasing physical distance between the Source and Recipients beyond 0.9 m provided minimal exposure reduction when oriented side-by-side. However, maintaining a physical distance of 1.8 m or more between the Source and a Recipient in the face-to-face orientation was critical”. A 2021 article published in the ASHRAE Journal discussed their modeling study with mannequins made to “inhale” and “exhale” aerosols in a modified classroom layout (7 feet separation between students and a 10 foot buffer separation between the instructor and seated students) found that exhaled aerosol density is stronger closer to the source, and that while evaluating various types of masks designed to cover the nose and mouth with the intent of providing protection for the wearer (inhalation) and for those in physical proximity to the wearer (exhalation), mask fitters or braces better enabled the mask to achieve full filtration potential consistently by reducing air leakage around the mask. Another 2021 study published in Science found that “effective ventilation and social distancing will reduce ambient virus concentrations and increase the effectiveness of face masks in containing the virus transmission”.
Remote and Virtual Options
Remote and virtual options are the highest level of physical distance, and, when you are in different physical environments from other households, you do not need to use other layers of protection. Although not all activities can be done remotely, increasing remote activities will reduce overall risks. Places that add remote options provide access and protection to those seeking such options, providing benefits to employees, patrons, and society as a whole.
Remote and Virtual options are becoming increasingly available, with use of online video platforms such as Zoom, Google Meet, and Slack allowing people to interact from any location.
Virtual schools, work from home jobs, telehealth, mobile care services, online ordering/delivery, and curbside pickup options are ways to reduce risks and exposures to COVID-19.
Hybrid options and flexibilities, also encourage better adherence to proper isolation guidance for people who are feeling ill, testing positive, and/or were recently exposed to COVID-19 by allowing them to work from home in those situations reducing impacts of absences on both the individual and group.
Individuals can choose to use remote options as alternatives to attending shared in-person spaces that are not implementing protections. This will not only keep them safe but will encourage those in charge of physical spaces to take the steps needed to make their spaces safer by using the above protections.
Supporting Layers: Testing And Isolating
Testing
Testing [9] can be used to screen for and pick up COVID-19 infections with varying degrees of accuracy depending on:
When the test is taken: Recent data shows viral loads peak on the fourth day after infection. Therefore, it is important to continue testing after exposure for at least four days, as earlier tests may miss picking up infections;
How often one tests: Accuracy improves with serial testing. The FDA recommends repeat testing at least 3 times at 48-hour intervals when asymptomatic, and 2 times separated by 48 hours when symptomatic;
Type of test taken: Molecular tests, such as polymerase chain reaction (PCR) tests are more accurate than Rapid Antigen Tests (RATs); Home molecular test kits are available (Lucira COVID, Lucira COVID+flu, or Metrix COVID test kits), which detect viral genetic material like PCR tests. These home molecular tests are more sensitive and accurate than antigen tests, but they are also more expensive (some are $25-50 per test or require the one-time purchase of an expensive reader);
Symptoms: Tests are more likely to pick up symptomatic cases than asymptomatic cases. (Note: Both asymptomatic and symptomatic people can be infectious).
How the sample is collected: Viral loads tend to rise in the throat before the nose, and collecting both nose and throat samples can significantly improve accuracy.
The age of the person: children and young adults have lower accuracy ratings than adults in some studies.
Other factors: type of comparator a test brand uses (BinaxNow comparator was not as accurate for Omicron than it was for Delta); timing of last vaccine or infection.
Catching COVID-19 on a test at onset has proven extremely difficult since many people are either pre-symptomatic or asymptomatic. The tests have worse accuracy with asymptomatic and presymptomatic infections despite the person being contagious.
Testing is valuable because identifying infections can assist with getting timely treatment as well as motivating people to isolate for the correct amount of time and therefore reducing transmissions. It is also good to confirm infections in case one develops long COVID later on.
However, because tests can miss and/or delay picking up many cases, they cannot rule out an infection or contagiousness. For this reason, masking should not be removed unless a regimen is followed to have that person enter your "bubble", which often requires quarantine isolation periods, and multiple tests, as symptoms may appear 2-14 days after exposure.
[9] Testing Accuracy/Infectiousness: Studies have found: ~63% of people don’t have symptoms when they are first infectious with the Omicron variant, and ~32% don’t ever develop symptoms even though they can infect others. According to a 2021 study in the Journal of Infectious Diseases, PCR tests are more accurate than RAT tests at both picking up asymptomatic or presymptomatic individuals before they can transmit the virus, thus mitigating spread, as well as identifying individuals at later stages of infection. They noted both test types should be done serially, at least every 3 days. A 2023 study on the performance of rapid antigen tests found accuracy was optimized when asymptomatic participants tested 3 times at 48-hour intervals and when symptomatic participants tested 2 times separated by 48 hours. Tests are more likely to pick up symptomatic cases than asymptomatic cases. In a 2022 study on the accuracy of RAT tests with Omicron variants in students ages 17-22 found that among symptomatic participants, RAT had a sensitivity of 77.8%; among asymptomatic patients, accuracy was only 39.2%. A 2023 study shows collecting both throat and nasal samples improved RAT accuracy by 15-21 percentage points, as Omicron viral loads rise in the throat before the nose. A2021 cohort study published in JAMA found that “individuals with COVID-19 were most infectious a few days before and after symptom onset.” However, according to data, rapid antigen tests often don't pick up COVID-19 infections until day 4. A2022 study on Omicron in asymptomatic individuals found low accuracy of RATs (20-27%) and also found PCRs accuracy was only 40-48% amongst asymptomatic individuals. They concluded that“SARS-CoV-2 self-testing has limited value for asymptomatic individuals wishing to protect vulnerable persons and may even lead to a false sense of security. One should be aware of this, and better informed about other prevention options, such as physical distancing or mask use, on the other hand, all evaluated self-tests were highly specific. Therefore, self-testing regardless of symptoms is useful in other public health contexts because every positive test captured reduces the number of subsequent exposures. The high SARS-CoV-2 infection rate within 10 days of a negative RT-PCR test that we found in our study emphasizes the importance of re-testing over time, especially when symptoms develop, to reduce missed infections as much as possible.” A study on the accuracy of PCR tests in children and young adults found “that nearly 90% of children had negative nasopharyngeal RT-PCR samples, yet they seroconverted 6 weeks later, confirming infection”. A 2023 study shows other complex factors such as the variant and type of comparator a test brand uses (BinaxNow comparator was not as accurate for Omicron than it was for Delta; other brands using different comparators were about the same accuracy); the person's immune, vaccination status, and timing of last vaccine or infection also may play a role on when a person tests positive.
A person (whether vaccinated or not) should test:
If you have symptoms, test immediately.
The top 5 symptoms reported with Omicron infections are:
Note: These symptoms look like typical cold, flu and/or allergy symptoms, so if you think you might have a cold or new allergies, test immediately.
Test 1: Test again 1-2 days later if the first test is negative. Assume you have something infectious, wear a mask and stay home when possible.
Test 2: If the rapid test result is negative, isolate/quarantine (wear a mask any time you have to be around others) and repeat the test in 1-2 days.
Test 3: If you still have symptoms after two negative rapid tests, test a third time with a rapid test or get a PCR test. A PCR test will pick up lower viral levels (which may be a characteristic of Omicron infections), so get a PCR test if you have symptoms and repeatedly negative rapid tests.
B. If you were exposed, test as soon as possible and repeat 3-5 days after the exposure. For better accuracy, test every 2 days for a total of 3-4 tests, even if you don’t have symptoms.
C. Before travel, gathering or returning to school/work, test right before traveling/gathering/return and repeat 3-5 days after.
The National Institute for Health (NIH) has developed a website test2treat.org to offer free COVID tests, virtual appointments, and treatments (if eligible).
PCRs are higher accuracy but more expensive, Rapid Antigen Tests are less expensive but less accurate. Home molecular test kits are also available (Lucira COVID, Lucira COVID+flu, Metrix, PlusLife, CueHealth), which detect viral genetic material like PCR tests.
Note: Most at-home tests can be safely used past the date on the box. Check to see if your COVID-19 tests’ expiration dates have been extended on the FDA’s At-Home COVID-19 Test page.
Isolating
It is important to isolate properly to prevent transmission of COVID-19. There has been considerable confusion and debate in public health messaging regarding when and how long to isolate for, despite science that has consistently supported a minimum 14-day isolation period [10].
The Gold Standard Isolation guidance states: After isolating 14 days, before ending isolation, both of the following conditions must also be met:
1- No symptoms for three days AND
2- Two sequential negative PCR tests spaced 24-hours apart (each test should include samples taken from two sources). {see above testing section for more information on using other tests}
The above gold standard provides strong assurance that SARS-COV2 transmission will not take place from identified cases.
[10] A minimum 14 day isolation period, is considered the gold standard for isolation and is necessary for infection control from COVID-19. A 2022 study showed that among the SARS-CoV-2 Omicron variant infected patients, viral shedding continues for more than 10 days in 13.5% of all cases and 11% in symptom-free cases. Researchers also showed that determining infectiousness by symptoms is not accurate: “In 19% of the cases, the duration of shedding was longer than the duration of the symptoms. On day 5, four patients declared no more symptoms, although viruses were isolated by the culture. The rate of viral shedding among symptom-free cases was 58% on day 7, whereas they were 11% on day 10 and 5% on day 14”, showing infectious virus shedding continued up to 2 days after symptom resolution. A 2023 study showed a significant amount of infectious virus was detected in the exhaled breath of COVID-positive people for 8 days regardless of vaccination status, and including asymptomatic and mild cases. A person could therefore be infectious longer than the CDC guidelines, even in mild and asymptomatic cases, or cases when symptoms are improving or have stopped.
The CDC’s 2024 updated guidance strays from the research, where they recommend that people stay home and away from others until at least 24 hours after both their symptoms are getting better overall, and they have not had a fever (and are not using fever-reducing medication) and “encourages added precaution over the next five days after time at home, away from others, is over.” The guidance admits that others may still be contagious, saying: "Since some people remain contagious beyond the “stay-at-home” period, a period of added precaution using prevention strategies, such as taking more steps for cleaner air, enhancing hygiene practices, wearing a well-fitting mask, keeping a distance from others, and/or getting tested for respiratory viruses can lower the chance of spreading respiratory viruses to others.” However, precautions such as one-way masking, air filtration, and even vaccination work best in settings with reduced viral load. CDC’s 2024 guidance will increase the number of contagious people in spaces, and reduce the effectiveness of precautions.
COVID-19 Isolation policies should support a minimum of 14-day isolation to reduce viral density in public spaces so that the other methods of infection prevention have a greater chance at preventing infection.
Supporting Layers: Vaccines
Vaccines [11] may reduce risks of severe disease, hospitalization and death during the acute phase of infection thus providing biological protection for the individual. However, their effectiveness wanes over time, they don’t prevent infection or transmission, and they do not prevent long COVID. Also not all people are or can be vaccinated (some decide not to vaccinate due to their own risk-benefit analysis, some have medical contraindications such as allergic reactions) and not all who get vaccinated are significantly protected, (e.g. the elderly or immune-compromised). Thus, it is important to wear a mask whether vaccinated or not to prevent infection and transmission.
Figure 9: Vaccines: A Back-Up Layer to Reduce Some Forms of Risk
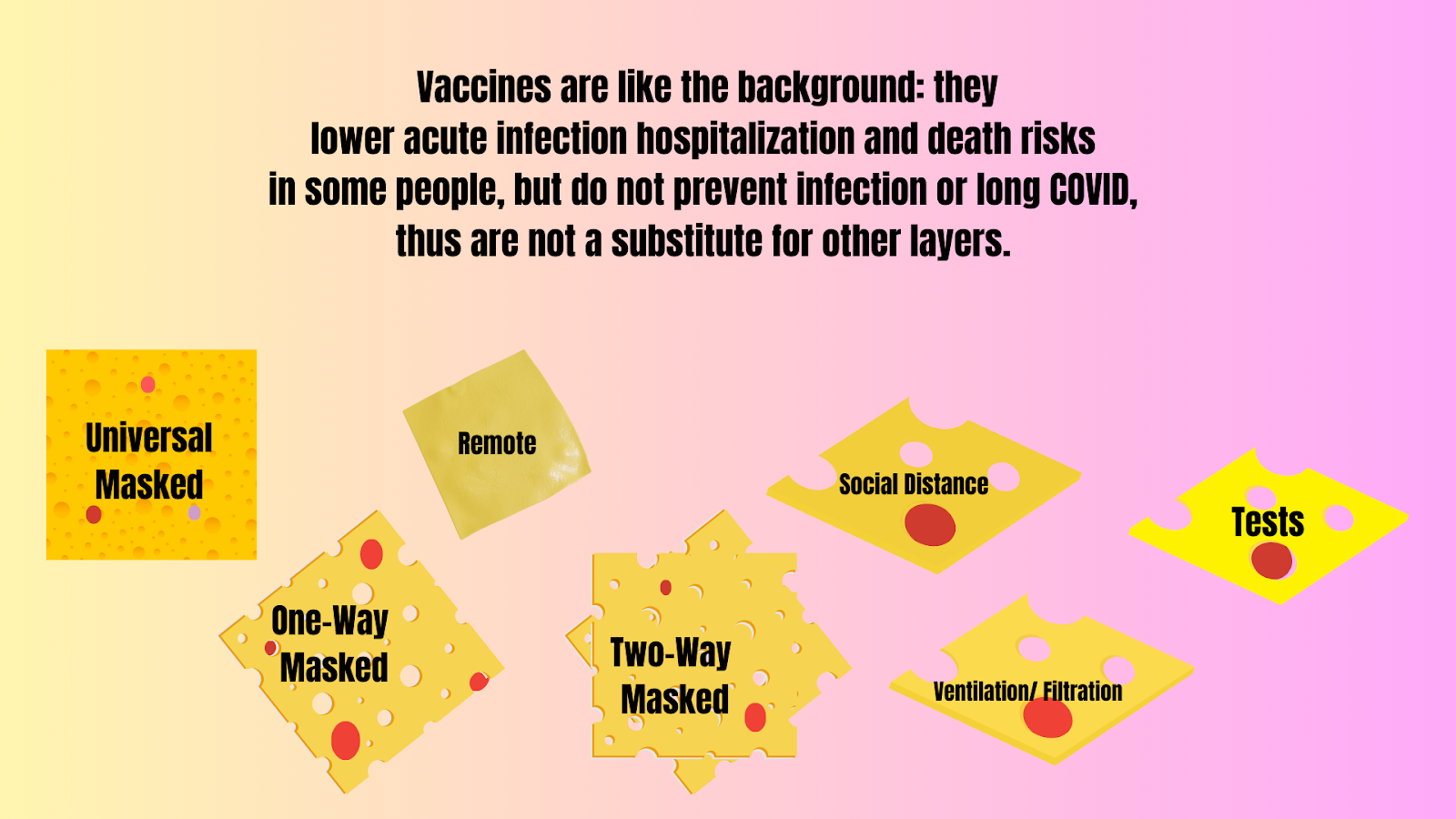
Vaccines are an additional layer to wearing a mask, not a substitution for it.
Individual responsibilities include staying educated about and up-to-date on vaccinations and available treatments, and seeking them when needed and appropriate, as well as maintaining other measures to prevent transmission.
[11] Vaccines: A 2022 study showed that 60-day vaccine efficacy of a second mRNA COVID-19 vaccine booster dose was 25.8% against infection, 60.1% against hospitalization, 89.6% against death, and 73.9% against the severe composite outcome of COVID-19–associated hospitalization or death. A 2023 study showed an estimated vaccine efficacy against hospitalization waned over time, showing 68% for a third dose 7 to 119 days after receipt, and 36% for a third dose 120 days or more after receipt. A 2024 study showed receipt of updated COVID-19 vaccine provided approximately 54% increased protection against symptomatic SARS-CoV-2 infection compared with no receipt of updated vaccine. A new 2024 study shows that the vaccine has been tied to a slight spike in certain conditions. Although the risks are much higher for infection from COVID-19, those who are able to shield and mask may weigh their risk benefit analysis differently. Vaccination does not prevent long COVID: Some studies show a modest reduction in long COVID amongst vaccinated individuals, but the reduction is not enough to lower risks to an acceptable level considering the nature of and lack of treatments for long COVID, and therefore is not considered a solution on its own. A 2022 study published in Nature, found a 15% reduction in long Covid amongst those vaccinated. The authors concluded that “vaccination before infection confers only partial protection in the post-acute phase of the disease; hence, reliance on it as a sole mitigation strategy may not optimally reduce long-term health consequences of SARS-CoV-2 infection.” A 2023 population-level analysis found vaccines reduced long COVID by 15-20%, with the authors concluding “Complementing vaccination campaigns with potential therapies, as well as further investing on prevention, might reduce the prevalence of long COVID and, consequently, should be considered for public health policies in the next future.” A 2023 Swedish study analysis found vaccine effectiveness against long COVID was 21% for one dose, 59% for 2 doses, and 73% for 3 or more doses, showing the importance of staying up-to-date on vaccinations, although it relied on diagnoses being made by primary care physicians in Sweden. A 2024 Lancet study found vaccines conferred 29-52% protection against long COVID. Barriers in defining, identifying, and diagnosing long COVID may be responsible for the variation in percentages for protective effect. Vaccine protection is not all or nothing: A 2023 study shows vaccines are much more effective in preventing transmission when the person inhales a smaller viral load. Masking can reduce inhaled viral load, which could in turn increase the vaccines’ ability to actually prevent infection.
Summary
In summary, it is important to not simply focus on using many layers, but to also pay attention to how these layers actually work and to choose complementary layers to provide true risk-reduction for you and others in the community. All are at risk for serious effects of COVID-19 and our actions affect those around us.
Using clear messaging about what really works is the first step in overcoming obstacles to technological development, related policies, and implementation, and to bringing these tools into our home, work, school, and business spaces.
For more information, visit World Health Network’s Guidelines for Individuals and Institutions.
For Information on School Safety see WHN’s Paths to Healthy Learning.
For information for Healthcare Professionals see Guidelines in Healthcare